La Organización Mundial de la Salud (OMS) publicó la “Lista Modelo OMS de Medicamentos Esenciales”, siendo actualizada cada dos años por un comité de expertos, compuesto por reconocidos especialistas del mundo académico, de investigación y de las profesiones médicas y farmacéuticas. Su última actualización fue celebrada entre el 27 y el 31 de marzo del 2017, en la sede de la OMS, en Ginebra, Suiza.
Su propósito es proporcionar una guía para la priorización de los medicamentos desde un perspectiva clínica y de salud pública. El trabajo duro comienza con los esfuerzos para asegurar que los medicamentos están realmente disponibles para los pacientes.
El número total en la lista se eleva a un total de 433 medicamentos considerados esenciales para responder a las necesidades más importantes de salud pública.
Entre los últimos cambios introducidos figuran nuevas recomendaciones sobre qué antibióticos se han de utilizar contra las infecciones comunes y cuáles se deben reservar para los casos más graves. Asimismo se han añadido medicamentos contra la infección por el VIH, la hepatitis C, la tuberculosis y la leucemia.
“La seguridad y eficacia de los medicamentos son aspectos esenciales de cualquier sistema de salud. Velar porque todas las personas tengan acceso a los medicamentos que requieran, cuando y donde los necesiten, es esencial para que los países avancen hacia el logro de la cobertura sanitaria universal”.
WHO Model List of Essential Medicines
20th List
(March 2017)
(Amended August 2017)
| 1. ANAESTHETICS, PREOPERATIVE MEDICINES AND MEDICAL GASES | |
| 1.1 General anaesthetics and oxygen | |
| 1.1.1 Inhalational medicines | |
| halothane | Inhalation. |
| isoflurane | Inhalation. |
| nitrous oxide | Inhalation. |
| oxygen | Inhalation (medical gas). |
| 1.1.2 Injectable medicines | |
| ketamine | Injection: 50 mg (as hydrochloride)/ mL in 10- mL vial. |
| propofol* | Injection: 10 mg/ mL; 20 mg/ mL.
* Thiopental may be used as an alternative depending on local availability and cost. |
| 1.2 Local anaesthetics | |
| o bupivacaine | Injection: 0.25%; 0.5% (hydrochloride) in vial.
Injection for spinal anaesthesia: 0.5% (hydrochloride) in 4- mL ampoule to be mixed with 7.5% glucose solution. |
| o lidocaine | Injection: 1%; 2% (hydrochloride) in vial.
Injection for spinal anaesthesia: 5% (hydrochloride) in 2- mL ampoule to be mixed with 7.5% glucose solution. Topical forms: 2% to 4% (hydrochloride). |
| lidocaine + epinephrine (adrenaline) | Dental cartridge: 2% (hydrochloride) + epinephrine 1:80 000.
Injection: 1%; 2% (hydrochloride or sulfate) + epinephrine 1:200 000 in vial. |
| Complementary List | |
| ephedrine | Injection: 30 mg (hydrochloride)/ mL in 1- mL ampoule.
(For use in spinal anaesthesia during delivery, to prevent hypotension). |
| 1.3 Preoperative medication and sedation for short-term procedures | |
| atropine | Injection: 1 mg (sulfate) in 1- mL ampoule. |
| o midazolam | Injection: 1 mg/ mL.
Oral liquid: 2 mg/ mL [c]. Tablet: 7.5 mg; 15 mg. |
| morphine | Injection: 10 mg (sulfate or hydrochloride) in 1- mL ampoule. |
| 1.4 Medical gases | |
| oxygen* | Inhalation
For use in the management of hypoxaemia. *No more than 30% oxygen should be used to initiate resuscitation of neonates less than or equal to 32 weeks of gestation. |
| 2. MEDICINES FOR PAIN AND PALLIATIVE CARE | |
| 2.1 Non-opioids and non-steroidal anti-inflammatory medicines (NSAIMs) | |
| acetylsalicylic acid | Suppository: 50 mg to 150 mg.
Tablet: 100 mg to 500 mg. |
| ibuprofen a | Oral liquid: 200 mg/5 mL.
Tablet: 200 mg; 400 mg; 600 mg. a Not in children less than 3 months. |
| paracetamol* | Oral liquid: 120 mg/5 mL; 125 mg/5 mL.
Suppository: 100 mg. Tablet: 100 mg to 500 mg. * Not recommended for anti-inflammatory use due to lack of proven benefit to that effect. |
| 2.2 Opioid analgesics | |
| codeine | Tablet: 30 mg (phosphate). |
| fentanyl* | Transdermal patch: 12 micrograms/hr; 25 micrograms/hr; 50
micrograms/hr; 75 micrograms/hr; 100 micrograms/hr *for the management of cancer pain |
| o morphine* | Granules (slow-release; to mix with water): 20 mg –200 mg (morphine sulfate).
Injection: 10 mg (morphine hydrochloride or morphine sulfate) in 1- mL ampoule. Oral liquid: 10 mg (morphine hydrochloride or morphine sulfate)/5 mL. Tablet (slow release): 10 mg–200mg (morphine hydrochloride or morphine sulfate). Tablet (immediate release): 10 mg (morphine sulfate). *Alternatives limited to hydromorphone and oxycodone |
| Complementary list | |
| methadone* | Tablet: 5 mg; 10 mg (as hydrochloride)
Oral liquid: 5mg/ 5mL; 10mg/ 5mL (as hydrochloride) Concentrate for oral liquid: 5 mg/ mL; 10mg/ mL (as hydrochloride) *For the management of cancer pain. |
| 2.3 Medicines for other common symptoms in palliative care | |
| amitriptyline | Tablet: 10 mg; 25 mg; 75 mg. |
| cyclizine [c] | Injection: 50 mg/ mL.
Tablet: 50 mg. |
| dexamethasone | Injection: 4 mg/ mL in 1- mL ampoule (as disodium phosphate salt).
Oral liquid: 2 mg/5 mL. Tablet: 2 mg [c]; 4 mg. |
| diazepam | Injection: 5 mg/ mL.
Oral liquid: 2 mg/5 mL. Rectal solution: 2.5 mg; 5 mg; 10 mg. Tablet: 5 mg; 10 mg. |
| docusate sodium | Capsule: 100 mg.
Oral liquid: 50 mg/5 mL. |
| fluoxetine a | Solid oral dosage form: 20 mg (as hydrochloride).
a >8 years. |
| haloperidol | Injection: 5 mg in 1‐ mL ampoule.
Oral liquid: 2 mg/ mL. Solid oral dosage form: 0.5 mg; 2mg; 5 mg. |
| hyoscine butylbromide | Injection: 20 mg/ mL. |
| hyoscine hydrobromide [c] | Injection: 400 micrograms/ mL; 600 micrograms/ mL.
Transdermal patches: 1 mg/72 hours. |
| lactulose [c] | Oral liquid: 3.1–3.7 g/5 mL. |
| loperamide | Solid oral dosage form: 2 mg. |
| metoclopramide | Injection: 5 mg (hydrochloride)/mL in 2‐mL ampoule.
Oral liquid: 5 mg/5 mL. Solid oral form: 10 mg (hydrochloride). |
| midazolam | Injection: 1 mg/ mL; 5 mg/ mL.
Solid oral dosage form: 7.5 mg; 15 mg. Oral liquid: 2mg/ mL [c]. |
| ondansetron [c] a | Injection: 2 mg base/ mL in 2- mL ampoule (as hydrochloride).
Oral liquid: 4 mg base/5 mL. Solid oral dosage form: Eq 4 mg base; Eq 8 mg base. a >1 month. |
| senna | Oral liquid: 7.5 mg/5 mL. |
| 3. ANTIALLERGICS AND MEDICINES USED IN ANAPHYLAXIS | |
| dexamethasone | Injection: 4 mg/ mL in 1- mL ampoule (as disodium phosphate salt). |
| epinephrine (adrenaline) | Injection: 1 mg (as hydrochloride or hydrogen tartrate) in 1- mL ampoule. |
| hydrocortisone | Powder for injection: 100 mg (as sodium succinate) in vial. |
| o loratadine * | Oral liquid: 1 mg/ mL.
Tablet: 10 mg. *There may be a role for sedating antihistamines for limited indications (EMLc). |
| o prednisolone | Oral liquid: 5 mg/ mL [c].
Tablet: 5 mg; 25 mg. |
| 4. ANTIDOTES AND OTHER SUBSTANCES USED IN POISONINGS | |
| 4.1 Non-specific | |
| charcoal, activated | Powder. |
| 4.2 Specific | |
| acetylcysteine | Injection: 200 mg/ mL in 10- mL ampoule.
Oral liquid: 10% [c]; 20% [c]. |
| atropine | Injection: 1 mg (sulfate) in 1- mL ampoule. |
| calcium gluconate | Injection: 100 mg/ mL in 10- mL ampoule. |
| methylthioninium chloride (methylene blue) | Injection: 10 mg/ mL in 10- mL ampoule. |
| naloxone | Injection: 400 micrograms (hydrochloride) in 1- mL ampoule. |
| penicillamine | Solid oral dosage form: 250 mg. |
| potassium ferric hexacyano-ferrate(II) – 2H2O(Prussian blue) | Powder for oral administration. |
| sodium nitrite | Injection: 30 mg/ mL in 10- mL ampoule. |
| sodium thiosulfate | Injection: 250 mg/ mL in 50- mL ampoule. |
| Complementary List | |
| deferoxamine | Powder for injection: 500 mg (mesilate) in vial. |
| dimercaprol | Injection in oil: 50 mg/ mL in 2- mL ampoule. |
| fomepizole | Injection: 5 mg/ mL (sulfate) in 20- mL ampoule or 1 g/ mL (base) in 1.5- mL ampoule. |
| sodium calcium edetate | Injection: 200 mg/ mL in 5- mL ampoule. |
| succimer | Solid oral dosage form: 100 mg. |
| 5. ANTICONVULSANTS/ANTIEPILEPTICS | |
| carbamazepine | Oral liquid: 100 mg/5 mL.
Tablet (chewable): 100 mg; 200 mg. Tablet (scored): 100 mg; 200 mg. |
| diazepam | Gel or rectal solution: 5 mg/ mL in 0.5 mL; 2- mL; 4- mL tubes. |
| lamotrigine* | Tablet: 25 mg; 50 mg; 100 mg; 200 mg.
Tablet (chewable, dispersible): 2 mg; 5 mg; 25 mg; 50 mg; 100 mg; 200 mg. *as adjunctive therapy for treatment-resistant partial or generalized seizures. |
| o lorazepam | Parenteral formulation: 2 mg/ mL in 1- mL ampoule; 4 mg/ mL in 1- mL ampoule. |
| magnesium sulfate* | Injection: 0.5g/ mL in 2- mL ampoule (equivalent to 1 g in 2 mL; 50% weight/volume); 0.5g/ mL in
10- mL ampoule (equivalent to 5 g in 10 mL; 50% weight/volume). * For use in eclampsia and severe pre-eclampsia and not for other convulsant disorders. |
| midazolam | Solution for oromucosal administration: 5 mg/mL; 10 mg/mL
Ampoule*: 1 mg/ mL; 10 mg/mL *for buccal administration when solution for oromucosal administration is not available |
| phenobarbital | Injection: 200 mg/ mL (sodium).
Oral liquid: 15 mg/5 mL. Tablet: 15 mg to 100 mg. |
| phenytoin | Injection: 50 mg/ mL in 5- mL vial (sodium salt).
Oral liquid: 25 mg to 30 mg/5 mL.* Solid oral dosage form: 25 mg; 50 mg; 100 mg (sodium salt). Tablet (chewable): 50 mg. * The presence of both 25 mg/5 mL and 30 mg/5 mL strengths on the same market would cause confusion in prescribing and dispensing and should be avoided. |
| valproic acid (sodium valproate) | Oral liquid: 200 mg/5 mL.
Tablet (crushable): 100 mg. Tablet (enteric-coated): 200 mg; 500 mg (sodium valproate). |
| Complementary List | |
| ethosuximide | Capsule: 250 mg.
Oral liquid: 250 mg/5 mL. |
| valproic acid (sodium valproate) | Injection: 100 mg/ mL in 4- mL ampoule; 100 mg/ mL in 10- mL ampoule. |
| 6. ANTI-INFECTIVE MEDICINES | |
| 6.1 Anthelminthics | |
| 6.1.1 Intestinal anthelminthics | |
| albendazole | Tablet (chewable): 400 mg. |
| ivermectin | Tablet (scored): 3 mg. |
| levamisole | Tablet: 50 mg; 150 mg (as hydrochloride). |
| mebendazole | Tablet (chewable): 100 mg; 500 mg. |
| niclosamide | Tablet (chewable): 500 mg. |
| praziquantel | Tablet: 150 mg; 600 mg. |
| pyrantel | Oral liquid: 50 mg (as embonate or pamoate)/ mL.
Tablet (chewable): 250 mg (as embonate or pamoate). |
| 6.1.2 Antifilarials | |
| albendazole | Tablet (chewable): 400 mg. |
| diethylcarbamazine | Tablet: 50 mg; 100 mg (dihydrogen citrate). |
| ivermectin | Tablet (scored): 3 mg. |
| 6.1.3 Antischistosomals and other antitrematode medicines | |
| praziquantel | Tablet: 600 mg. |
| triclabendazole | Tablet: 250 mg. |
| Complementary List | |
| oxamniquine* | Capsule: 250 mg.
Oral liquid: 250 mg/5 mL. * Oxamniquine is listed for use when praziquantel treatment fails. |
6.2 Antibacterials
To assist in the development of tools for antibiotic stewardship at local, national and global levels and to reduce antimicrobial resistance, three different categories were developed – ACCESS, WATCH and RESERVE groups.
Group 1 – KEY ACCESS ANTIBIOTICS
To improve both access and clinical outcomes antibiotics that were first or second choice antibiotics in at least one of the reviewed syndromes are designated as key ACCESS antibiotics, emphasizing their role as the antibiotics that should be widely available, affordable and quality-assured. ACCESS antibiotics are listed below. Selected ACCESS antibiotics may also be included in the WATCH group.
| 6.2.1 Beta-lactam medicines | 6.2.2 Other antibacterials | ||
| amoxicillin | cefotaxime* | amikacin | gentamicin |
| amoxicillin + clavulanic acid | ceftriaxone* | azithromycin* | metronidazole |
| ampicillin | cloxacillin | chloramphenicol | nitrofurantoin |
| benzathine benzylpenicillin | phenoxymethylpenicillin | ciprofloxacin* | spectinomycin (EML only) |
| benzylpenicillin | piperacillin + tazobactam* | clarithromycin* | sulfamethoxazole + trimethoprim |
| cefalexin | procaine benzyl penicillin | clindamycin | vancomycin (oral)* |
| cefazolin | meropenem* | doxycycline | vancomycin (parenteral)* |
| cefixime* | |||
Italics = complementary list
*Watch group antibiotics included in the EML/EMLc only for specific, limited indications
The 2017 Expert Committee identified the following antibiotics or antibiotic classes that should be the subject of a specific stewardship focus. Antibiotics or antibiotic classes in these groups are designated accordingly in the EML/EMLc. The “WATCH” and “RESERVE” stewardship groups could assist in activities such as local, national and global monitoring of use; development of guidelines and educational activities.
Group 2 – WATCH GROUP ANTIBIOTICS
This group includes antibiotic classes that have higher resistance potential and so are recommended as first or second choice treatments only for a specific, limited number of indications. These medicines should be prioritized as key targets of stewardship programs and monitoring.
This group includes most of the highest priority agents among the Critically Important Antimicrobials for Human Medicine1 and/or antibiotics that are at relatively high risk of selection of bacterial resistance.
| Watch group antibiotics |
| Quinolones and fluoroquinolones
e.g. ciprofloxacin, levofloxacin, moxifloxacin, norfloxacin |
| 3rd-generation cephalosporins (with or without beta-lactamase inhibitor)
e.g. cefixime, ceftriaxone, cefotaxime, ceftazidime |
| Macrolides
e.g. azithromycin, clarithromycin, erythromycin |
| Glycopeptides
e.g. teicoplanin, vancomycin |
| Antipseudomonal penicillins + beta-lactamase inhibitor
e.g. piperacillin-tazobactam |
| Carbapenems
e.g. meropenem, imipenem + cilastatin |
| Penems
e.g. faropenem |
1 https://apps.who.int/iris/bitstream/10665/251715/1/9789241511469-eng.pdf?ua=1
| Group 3 – RESERVE GROUP ANTIBIOTICS
This group includes antibiotics that should be treated as “last resort” options that should be accessible, but whose use should be tailored to highly specific patients and settings, when all alternatives have failed (e.g., serious, life-threatening infections due to multi-drug resistant bacteria). These medicines could be protected and prioritized as key targets of national and international stewardship programs involving monitoring and utilization reporting, to preserve their effectiveness. |
||
| 6.2.1 Beta-lactam medicines | ||
| Powder for oral liquid: 125 mg (as trihydrate)/5 mL; 250 mg (as trihydrate)/5 mL [c]. | ||
| Solid oral dosage form: 250 mg; 500 mg (as trihydrate). | ||
| Powder for injection: 250 mg; 500 mg; 1 g (as sodium) in vial. | ||
| FIRST CHOICE | SECOND CHOICE | |
| – community acquired pneumonia (mild to | – acute bacterial meningitis | |
| amoxicillin | moderate)
– community acquired pneumonia (severe) [c] – complicated severe acute malnutrition [c] |
|
| – exacerbations of COPD | ||
| – lower urinary tract infections | ||
| – otitis media | ||
| – pharyngitis
– sepsis in neonates and children [c] |
||
| – sinusitis
– uncomplicated severe acute malnutrition [c] |
||
| amoxicillin + clavulanic acid | Oral liquid: 125 mg amoxicillin + 31.25 mg clavulanic acid/5 mL AND 250 mg amoxicillin + 62.5 mg clavulanic acid/5 mL [c].
Tablet: 500 mg (as trihydrate) + 125 mg (as potassium salt). Powder for injection: 500 mg (as sodium) + 100 mg (as potassium salt); 1000 mg (as sodium) + 200 mg (as potassium salt) in vial. |
|
| FIRST CHOICE
– community acquired pneumonia (severe) [c] – complicated intraabdominal infections (mild to moderate) – exacerbations of COPD – hospital acquired pneumonia – low-risk febrile neutropenia – lower urinary tract infections – sinusitis – skin and soft tissue infections |
SECOND CHOICE
– bone and joint infections – community-acquired pneumonia (mild to moderate) – community acquired pneumonia (severe) – otitis media |
|
| ampicillin | Powder for injection: 500 mg; 1 g (as sodium salt) in vial. | |
| FIRST CHOICE
– community acquired pneumonia (severe) [c] – complicated severe acute malnutrition [c] – sepsis in neonates and children [c] |
SECOND CHOICE
– acute bacterial meningitis |
|
| benzathine benzylpenicillin | Powder for injection: 900 mg benzylpenicillin (= 1.2 million IU) in 5- mL vial
[c]; 1.44 g benzylpenicillin (= 2.4 million IU) in 5- mL vial. |
|
| FIRST CHOICE
– syphilis |
SECOND CHOICE | |
| benzylpenicillin | Powder for injection: 600 mg (= 1 million IU); 3 g (= 5 million IU) (sodium or
potassium salt) in vial. |
|
| FIRST CHOICE
-community acquired pneumonia (severe) [c] – complicated severe acute malnutrition [c] – sepsis in neonates and children [c] – syphilis |
SECOND CHOICE
– acute bacterial meningitis[c] |
|
| cefalexin | Powder for reconstitution with water: 125 mg/5 mL; 250 mg/5 mL (anhydrous).
Solid oral dosage form: 250 mg (as monohydrate). |
|
| FIRST CHOICE | SECOND CHOICE
– exacerbations of COPD – pharyngitis – skin and soft tissue infections |
|
| cefazolin* a | Powder for injection: 1 g (as sodium salt) in vial.
* also indicated for surgical prophylaxis. a >1 month. |
|
| FIRST CHOICE | SECOND CHOICE
– bone and joint infections |
|
| cefixime WATCH GROUP | Capsule or tablet: 200 mg; 400 mg (as trihydrate).
Powder for oral liquid: 100 mg /5 mL [c] |
|
| FIRST CHOICE | SECOND CHOICE
– acute invasive bacterial diarrhoea / dysentery – Neisseria gonorrhoeae |
|
| cefotaxime* WATCH GROUP | Powder for injection: 250 mg per vial (as sodium salt)
* 3rd generation cephalosporin of choice for use in hospitalized neonates. |
|
| FIRST CHOICE
– acute bacterial meningitis -community acquired pneumonia (severe) – complicated intraabdominal infections (mild to moderate) – complicated intrabdominal infections (severe) – hospital acquired pneumonia -pyelonephritis or prostatitis (severe) |
SECOND CHOICE
– bone and joint infections -pyelonephritis or prostatitis (mild to moderate) – sepsis in neonates and children [c] |
|
| ceftriaxone* a
WATCH GROUP |
Powder for injection: 250 mg; 1 g (as sodium salt) in vial.
* Do not administer with calcium and avoid in infants with hyperbilirubinaemia. a >41 weeks corrected gestational age. |
|
| FIRST CHOICE
– acute bacterial meningitis -community acquired pneumonia (severe) – complicated intraabdominal infections (mild to moderate) – complicated intrabdominal infections (severe) – hospital acquired pneumonia – Neisseria gonorrhoeae -pyelonephritis or prostatitis (severe) |
SECOND CHOICE
– acute invasive bacterial diarrhoea / dysentery – bone and joint infections – pyelonephritis or prostatitis (mild to moderate) – sepsis in neonates and children [c] |
|
| o cloxacillin* | Capsule: 500 mg; 1 g (as sodium salt).
Powder for injection: 500 mg (as sodium salt) in vial. Powder for oral liquid: 125 mg (as sodium salt)/5 mL. *cloxacillin, dicloxacillin and flucloxacillin are preferred for oral administration due to better bioavailability. |
|
| FIRST CHOICE
– bone and joint infections – skin and soft tissue infections |
SECOND CHOICE
– sepsis in neonates and children [c] |
|
| phenoxymethylpenicillin | Powder for oral liquid: 250 mg (as potassium salt)/5 mL.
Tablet: 250 mg (as potassium salt). |
|||
| FIRST CHOICE
– community acquired pneumonia (mild to moderate) – pharyngitis |
SECOND CHOICE | |||
| piperacillin + tazobactam WATCH GROUP | Powder for injection: 2 g (as sodium salt) + 250 mg (as sodium salt); 4 g (as sodium salt) + 500 mg (as sodium salt) in vial | |||
| FIRST CHOICE
– complicated intraabdominal infections (severe) – high-risk febrile neutropenia – hospital acquired pneumonia |
SECOND CHOICE | |||
| procaine benzylpenicillin* | Powder for injection: 1 g (=1 million IU); 3 g (=3 million IU) in vial.
* Procaine benzylpenicillin is not recommended as first-line treatment for neonatal sepsis except in settings with high neonatal mortality, when given by trained health workers in cases where hospital care is not achievable. |
|||
| FIRST CHOICE
– syphilis [c] |
SECOND CHOICE
– syphilis |
|||
| Complementary List | ||||
| ceftazidime
WATCH GROUP |
Powder for injection: 250 mg or 1 g (as pentahydrate) in vial. | |||
| meropenem* a
WATCH GROUP |
Powder for injection: 500 mg (as trihydrate); 1 g (as trihydrate) in vial
a >3 months. *imipenem + cilastatin is an alternative except for acute bacterial meningitis where meropenem is preferred. |
|||
| FIRST CHOICE | SECOND CHOICE
– acute bacterial meningitis in neonates [c] – complicated intraabdominal infections (severe) – high-risk febrile neutropenia |
|||
| Complementary List – RESERVE GROUP | ||||
| aztreonam | Powder for injection: 1 g; 2 g in vial | |||
| fifth generation cephalosporins
(with or without beta-lactamase inhibitor) e.g, ceftaroline |
Powder for injection: 400 mg; 600 mg (as fosamil) in vial | |||
| fourth generation cephalosporins
(with or without beta-lactamase inhibitor) e.g., cefepime |
Powder for injection: 500 mg; 1g; 2g (as hydrochloride) in vial | ||
| 6.2.2 Other antibacterials | |||
| amikacin | Injection: 250 mg (as sulfate)/mL in 2- mL vial | ||
| FIRST CHOICE
-pyelonephritis or prostatitis (severe) |
SECOND CHOICE
– high-risk febrile neutropenia – sepsis in neonates and children [c] |
||
| azithromycin* WATCH GROUP | Capsule: 250 mg; 500 mg (anhydrous).
Oral liquid: 200 mg/5 mL. * also listed for single-dose treatment of trachoma and yaws. |
||
| FIRST CHOICE
– Chlamydia trachomatis – cholera [c] – Neisseria gonorrhoeae |
SECOND CHOICE
– acute invasive bacterial diarrhoea / dysentery – Neisseria gonorrhoeae |
||
| chloramphenicol | Capsule: 250 mg.
Oily suspension for injection*: 0.5 g (as sodium succinate)/ mL in 2- mL ampoule. * Only for the presumptive treatment of epidemic meningitis in children older than 2 years and in adults. Oral liquid: 150 mg (as palmitate)/5 mL. Powder for injection: 1 g (sodium succinate) in vial. |
||
| FIRST CHOICE | SECOND CHOICE
– acute bacterial meningitis |
||
| ciprofloxacin WATCH GROUP | Oral liquid: 250 mg/5 mL (anhydrous) [c].
Solution for IV infusion: 2 mg/ mL (as hyclate) [c]. Tablet: 250 mg (as hydrochloride). |
||
| FIRST CHOICE
– acute invasive bacterial diarrhoea / dysentery – low-risk febrile neutropenia – pyelonephritis or prostatitis (mild to moderate) |
SECOND CHOICE
-cholera – complicated intraabdominal infections (mild to moderate) |
||
| clarithromycin*† WATCH GROUP | Solid oral dosage form: 500 mg.
Powder for oral liquid: 125 mg/5 mL; 250 mg/5 mL Powder for injection: 500 mg in vial *erythromycin may be an alternative. †clarithromycin is also listed for use in combination regimens for eradication of H. pylori in adults. |
|
| FIRST CHOICE
-community acquired pneumonia (severe) |
SECOND CHOICE
– pharyngitis |
|
| clindamycin | Capsule: 150 mg (as hydrochloride).
Injection: 150 mg (as phosphate)/ mL. Oral liquid: 75 mg/5 mL (as palmitate) [c]. |
|
| FIRST CHOICE | SECOND CHOICE
– bone and joint infections |
|
| doxycycline a | Oral liquid: 25 mg/5 mL [c]; 50 mg/5 mL (anhydrous) [c].
Solid oral dosage form: 50 mg [c]; 100 mg (as hyclate). Powder for injection: 100 mg in vial a Use in children <8 years only for life-threatening infections when no alternative exists. |
|
| FIRST CHOICE
– Chlamydia trachomatis – cholera |
SECOND CHOICE
– cholera [c] -community acquired pneumonia (mild to moderate) – exacerbations of COPD |
|
| gentamicin | Injection: 10 mg; 40 mg (as sulfate)/ mL in 2- mL vial. | |
| FIRST CHOICE
– community acquired pneumonia (severe) [c] – complicated severe acute malnutrition [c] – sepsis in neonates and children [c] |
SECOND CHOICE
– Neisseria gonorrhoeae |
|
| metronidazole | Injection: 500 mg in 100- mL vial.
Oral liquid: 200 mg (as benzoate)/5 mL. Suppository: 500 mg; 1 g. Tablet: 200 mg to 500 mg. |
|
| FIRST CHOICE
– C. difficile infection – complicated intraabdominal infections (mild to moderate) – complicated intrabdominal infections (severe) – Trichomonas vaginalis |
SECOND CHOICE
– complicated intraabdominal infections (mild to moderate) |
||
| nitrofurantoin | Oral liquid: 25 mg/5 mL [c].
Tablet: 100 mg. |
||
| FIRST CHOICE
– lower urinary tract infections |
SECOND CHOICE | ||
| spectinomycin | Powder for injection: 2 g (as hydrochloride) in vial. | ||
| FIRST CHOICE | SECOND CHOICE
– Neisseria gonorrhoeae |
||
| sulfamethoxazole + trimethoprim* | Injection:
80 mg + 16 mg/ mL in 5- mL ampoule; 80 mg + 16 mg/ mL in 10- mL ampoule. Oral liquid: 200 mg + 40 mg/5 mL. Tablet: 100 mg + 20 mg; 400 mg + 80 mg; 800 mg + 160 mg. *single agent trimethoprim may be an alternative for lower urinary tract infection. |
||
| FIRST CHOICE
– lower urinary tract infections |
SECOND CHOICE
– acute invasive diarrhoea / bacterial dysentery |
||
| vancomycin WATCH GROUP | Capsule: 125 mg; 250 mg (as hydrochloride). | ||
| SECOND CHOICE
– C. difficile infection |
|||
| Complementary List | |||
| vancomycin WATCH GROUP | Powder for injection: 250 mg (as hydrochloride) in vial. | ||
| FIRST CHOICE | SECOND CHOICE
-high-risk febrile neutropenia |
||
| Complementary List – RESERVE GROUP | |||
| daptomycin | Powder for injection: 350 mg; 500 mg in vial | ||
| fosfomycin | Powder for injection: 2 g; 4 g (as sodium) in vial | ||
| oxazolindinones e.g., linezolid | Injection for intravenous administration: 2 mg/ mL in 300 mL bag.
Powder for oral liquid: 100 mg/5 mL. Tablet: 400 mg; 600 mg. |
|
| polymyxins
e.g., colistin |
Powder for injection: 1 million I.U. (as colistemethate sodium) in vial | |
| tigecycline | Powder for injection: 50 mg in vial | |
| 6.2.3 Antileprosy medicines | ||
| Medicines used in the treatment of leprosy should never be used except in combination. Combination therapy is essential to prevent the emergence of drug resistance. Colour-coded blister packs (MDT blister packs) containing standard two-medicine (paucibacillary leprosy) or three-medicine (multibacillary leprosy) combinations for adult and childhood leprosy should be used. MDT blister packs can be supplied free of charge through WHO. | ||
| clofazimine | Capsule: 50 mg; 100 mg. | |
| dapsone | Tablet: 25 mg; 50 mg; 100 mg. | |
| rifampicin | Solid oral dosage form: 150 mg; 300 mg. | |
| 6.2.4 Antituberculosis medicines
WHO recommends and endorses the use of fixed-dose combinations and the development of appropriate new fixed-dose combinations, including modified dosage forms, non-refrigerated products and paediatric dosage forms of assured pharmaceutical quality. |
||
| ethambutol | Oral liquid: 25 mg/ mL [c].
Tablet: 100 mg to 400 mg (hydrochloride). |
|
| ethambutol + isoniazid | Tablet: 400 mg + 150 mg. | |
| ethambutol + isoniazid + pyrazinamide + rifampicin | Tablet: 275 mg + 75 mg + 400 mg + 150 mg. | |
| ethambutol + isoniazid + rifampicin | Tablet: 275 mg + 75 mg + 150 mg. | |
| isoniazid | Oral liquid: 50 mg/5 mL [c].
Tablet: 100 mg to 300 mg. Tablet (scored): 50 mg. |
|
| isoniazid + pyrazinamide + rifampicin | Tablet:
75 mg + 400 mg + 150 mg. 150 mg + 500 mg + 150 mg (For intermittent use three times weekly). Tablet (dispersible): 50 mg + 150 mg + 75 mg [c]. |
|
| isoniazid + rifampicin | Tablet:
75 mg + 150 mg; 150 mg + 300 mg. 60 mg + 60 mg (For intermittent use three times weekly). 150 mg + 150 mg (For intermittent use three times weekly). Tablet (dispersible): 50 mg + 75 mg [c]. |
|
| pyrazinamide | Oral liquid: 30 mg/ mL [c].
Tablet: 400 mg. Tablet (dispersible): 150 mg. Tablet (scored): 150 mg. |
| rifabutin | Capsule: 150 mg.*
* For use only in patients with HIV receiving protease inhibitors. |
| rifampicin | Oral liquid: 20 mg/ mL [c].
Solid oral dosage form: 150 mg; 300 mg. |
| rifapentine* | Tablet: 150 mg
*For treatment of latent TB infection (LTBI) only |
| Complementary List | |
| Reserve second-line drugs for the treatment of multidrug-resistant tuberculosis (MDR-TB) should be used in specialized centres adhering to WHO standards for TB control. | |
| amikacin | Powder for injection: 100 mg; 500 mg; 1 g (as sulfate) in vial. |
| bedaquiline | Tablet: 100 mg. |
| capreomycin | Powder for injection: 1 g (as sulfate) in vial. |
| clofazimine | Capsule: 50 mg; 100 mg. |
| cycloserine* | Solid oral dosage form: 250 mg.
*Terizidone may be an alternative |
| delamanid a | Tablet: 50 mg.
a >6 years |
| ethionamide* | Tablet: 125 mg; 250 mg.
*Protionamide may be an alternative. |
| kanamycin | Powder for injection: 1 g (as sulfate) in vial. |
| levofloxacin | Tablet: 250mg; 500 mg; 750 mg. |
| linezolid | Injection for intravenous administration: 2 mg/ mL in 300 mL bag.
Powder for oral liquid: 100 mg/5 mL. Tablet: 400 mg; 600 mg. |
| moxifloxacin | Tablet: 400 mg. |
| p-aminosalicylic acid | Granules: 4 g in sachet.
Tablet: 500 mg. |
| streptomycin [c] | Powder for injection: 1 g (as sulfate) in vial. |
| 6.3 Antifungal medicines | |
| amphotericin B | Powder for injection: 50 mg in vial (as sodium deoxycholate or
liposomal complex). |
| clotrimazole | Vaginal cream: 1%; 10%.
Vaginal tablet: 100 mg; 500 mg. |
| fluconazole | Capsule: 50 mg.
Injection: 2 mg/ mL in vial. Oral liquid: 50 mg/5 mL. |
| flucytosine | Capsule: 250 mg.
Infusion: 2.5 g in 250 mL. |
| griseofulvin | Oral liquid: 125 mg/5 mL [c].
Solid oral dosage form: 125 mg; 250 mg. |
| itraconazole* | Capsule: 100 mg.
Oral liquid: 10 mg/mL. * For treatment of chronic pulmonary aspergillosis, histoplasmosis, sporotrichosis, paracoccidiodomycosis, mycoses caused by T. marneffei and chromoblastomycosis; and prophylaxis of histoplasmosis and infections caused by T. marneffei in AIDS patients. |
| nystatin | Lozenge: 100 000 IU.
Oral liquid: 50 mg/5 mL [c]; 100 000 IU/ mL [c]. Pessary: 100 000 IU. Tablet: 100 000 IU; 500 000 IU. |
| voriconazole* | Tablet: 50 mg; 200 mg
Powder for injection: 200 mg in vial Powder for oral liquid: 40 mg/mL *For treatment of chronic pulmonary aspergillosis and acute invasive aspergillosis. |
| Complementary List | |
| potassium iodide | Saturated solution. |
| 6.4 Antiviral medicines | |
| 6.4.1 Antiherpes medicines | |
| o aciclovir | Oral liquid: 200 mg/5 mL [c].
Powder for injection: 250 mg (as sodium salt) in vial. Tablet: 200 mg. |
| 6.4.2 Antiretrovirals | |
| Based on current evidence and experience of use, medicines in the following three classes of antiretrovirals are included as essential medicines for treatment and prevention of HIV (prevention of mother-to-child transmission, pre-exposure prophylaxsis (where indicated) and post-exposure prophylaxis). WHO emphasizes the importance of using these products in accordance with global and national guidelines. WHO recommends and endorses the use of fixed-dose combinations and the development of appropriate new fixed-dose combinations, including modified dosage forms, non-refrigerated products and paediatric dosage forms of assured pharmaceutical quality.
Scored tablets can be used in children and therefore can be considered for inclusion in the listing of tablets, provided that adequate quality products are available. |
|
| 6.4.2.1 Nucleoside/Nucleotide reverse transcriptase inhibitors | |
| abacavir (ABC) | Tablet: 300 mg (as sulfate).
Tablet (dispersible, scored): 60 mg (as sulfate) [c]. |
| lamivudine (3TC) | Oral liquid: 50 mg/5 mL [c].
Tablet: 150 mg. |
| tenofovir disoproxil fumarate† (TDF) | Tablet: 300 mg (tenofovir disoproxil fumarate – equivalent to 245 mg tenofovir disoproxil).
†also indicated for pre-exposure prophylaxis. |
| zidovudine (ZDV or AZT) | Capsule: 250 mg.
Oral liquid: 50 mg/5 mL. Solution for IV infusion injection: 10 mg/ mL in 20- mL vial. Tablet: 300 mg. Tablet (dispersible, scored): 60 mg [c]. |
| 6.4.2.2 Non-nucleoside reverse transcriptase inhibitors | |
| efavirenz (EFV or EFZ) a | Tablet: 200 mg (scored); 600 mg.
a >3 years or >10 kg weight. |
| nevirapine (NVP) a | Oral liquid: 50 mg/5 mL.
Tablet: 50 mg (dispersible); 200 mg. a> 6 weeks |
| 6.4.2.3 Protease inhibitors | |
| Selection of protease inhibitor(s) from the Model List will need to be determined by each country after consideration of international and national treatment guidelines and experience. Ritonavir is recommended for use in combination as a pharmacological booster, and not as an antiretroviral in its own right. All other protease inhibitors should be used in boosted forms (e.g. with ritonavir). | |
| atazanavir a | Solid oral dosage form: 100 mg; 300 mg (as sulfate).
a >25 kg. |
| atazanavir + ritonavir | Tablet (heat stable): 300 mg (as sulfate) + 100 mg. |
| darunavir a | Tablet: 75 mg; 400 mg; 600 mg; 800 mg
a >3 years |
| lopinavir + ritonavir (LPV/r) | Oral liquid: 400 mg + 100 mg/5 mL.
Tablet (heat stable): 100 mg + 25 mg; 200 mg + 50 mg. Capsule containing oral pellets: 40 mg + 10 mg [c]. |
| ritonavir | Oral liquid: 400 mg/5 mL.
Tablet (heat stable): 25 mg; 100 mg. |
| 6.4.2.4 Integrase inhibitors | |
| dolutegravir | Tablet: 50 mg |
| raltegravir* | Tablet (chewable): 25 mg; 100 mg.
Tablet: 400 mg *for use in pregnant women and in second-line regimens in accordance with WHO treatemnt guidelines. |
| FIXED-DOSE COMBINATIONS | |
| abacavir + lamivudine | Tablet (dispersible, scored): 60 mg (as sulfate) + 30 mg; 120 mg (as sulfate) + 60 mg. |
| efavirenz + emtricitabine* + tenofovir | Tablet: 600 mg + 200 mg + 300 mg (disoproxil fumarate equivalent to 245 mg tenofovir disoproxil).
*Emtricitabine (FTC) is an acceptable alternative to 3TC, based on knowledge of the pharmacology, the resistance patterns and clinical trials of antiretrovirals. |
| efavirenz + lamivudine + tenofovir | Tablet: 400 mg + 300 mg + 300 mg (disoproxil fumarate equivalent to 245 mg tenofovir disoproxil) |
| emtricitabine* + tenofovir† | Tablet: 200 mg + 300 mg (disoproxil fumarate equivalent to 245 mg tenofovir disoproxil).
*Emtricitabine (FTC) is an acceptable alternative to 3TC, based on knowledge of the pharmacology, the resistance patterns and clinical trials of antiretrovirals. † combination also indicated for pre-exposure prophylaxis |
| lamivudine + nevirapine + zidovudine | Tablet: 30 mg + 50 mg + 60 mg [c]; 150 mg + 200 mg + 300 mg. |
| lamivudine + zidovudine | Tablet: 30 mg + 60 mg [c]; 150 mg + 300 mg. |
| 6.4.2.5 Medicines for prevention of HIV-related opportunistic infections | |
| isoniazid + pyridoxine + sulfamethoxazole + trimethoprim | Tablet (scored): 300 mg + 25 mg + 800 mg + 160 mg |
| 6.4.3 Other antivirals | |
| ribavirin* | Injection for intravenous administration: 800 mg and 1 g in 10- mL phosphate buffer solution.
Solid oral dosage form: 200 mg; 400 mg; 600 mg. * For the treatment of viral haemorrhagic fevers |
| valganciclovir* | Tablet: 450 mg.
*For the treatment of cytomegalovirus retinitis (CMVr). |
| Complementary list | |
| oseltamivir* | Capsule: 30 mg; 45 mg; 75 mg (as phosphate).
Oral powder: 12 mg/ mL. * severe illness due to confirmed or suspected influenza virus infection in critically ill hospitalized patients |
| 6.4.4 Antihepatitis medicines | |
| 6.4.4.1 Medicines for hepatitis B | |
| 6.4.4.1.1 Nucleoside/Nucleotide reverse transcriptase inhibitors | |
| entecavir | Oral liquid: 0.05 mg/ mL
Tablet: 0.5 mg; 1 mg |
| tenofovir disoproxil fumarate (TDF) | Tablet: 300 mg (tenofovir disoproxil fumarate – equivalent to 245 mg tenofovir disoproxil). |
| 6.4.4.2 Medicines for hepatitis C | |
| Based on current evidence, medicines in the following classes of direct acting antiviral medicines are included as essential medicines for treatment of hepatitis C virus infection. WHO guidelines recommend specific combination therapy utilizing medicines from different classes. | |
| 6.4.4.2.1 Nucleotide polymerase inhibitors | |
| sofosbuvir | Tablet: 400 mg |
| 6.4.4.2.2 Protease inhibitors | |
| simeprevir | Capsule 150 mg |
| 6.4.4.2.3 NS5A inhibitors | |
| daclatasvir | Tablet: 30 mg; 60 mg (as hydrochloride) |
| 6.4.4.2.4 Non-nucleoside polymerase inhibitors | |
| dasabuvir | Tablet: 250 mg |
| 6.4.4.2.5 Other antivirals | |
| ribavirin* | Injection for intravenous administration: 800 mg and 1 g in 10- mL phosphate buffer solution.
Solid oral dosage form: 200 mg; 400 mg; 600 mg. * For the treatment of hepatitis C, in combination with peginterferon and/or direct acting anti-viral medicines |
| Complementary List | |
| pegylated interferon alfa (2a or 2b) * | Vial or prefilled syringe:
180 micrograms (peginterferon alfa-2a), 80 microgram, 100 microgram (peginterferon alfa-2b). * To be used in combination with ribavirin. |
| FIXED-DOSE COMBINATIONS
Alternative combinations of DAAs from different pharmacological classes are possible. |
|
| ledipasvir + sofosbuvir | Tablet: 90 mg + 400 mg. |
| ombitasvir + paritaprevir + ritonavir | Tablet: 12.5 mg + 75 mg + 50 mg |
| sofosbovir + velpatasvir | Tablet: 400 mg + 100 mg |
| 6.5 Antiprotozoal medicines | |
| 6.5.1 Antiamoebic and antigiardiasis medicines | |
| diloxanide a | Tablet: 500 mg (furoate).
a >25 kg. |
| o metronidazole | Injection: 500 mg in 100- mL vial.
Oral liquid: 200 mg (as benzoate)/5 mL. Tablet: 200 mg to 500 mg. |
| 6.5.2 Antileishmaniasis medicines | |
| amphotericin B | Powder for injection: 50 mg in vial (as sodium deoxycholate or
liposomal complex). |
| miltefosine | Solid oral dosage form: 10 mg; 50 mg. |
| paromomycin | Solution for intramuscular injection: 750 mg of paromomycin
base (as the sulfate). |
| sodium stibogluconate or meglumine antimoniate | Injection: 100 mg/ mL, 1 vial = 30 mL or 30%, equivalent to approximately 8.1% antimony (pentavalent) in 5- mL ampoule. |
| 6.5.3 Antimalarial medicines | |
| 6.5.3.1 For curative treatment | |
| Medicines for the treatment of P. falciparum malaria cases should be used in combination. The list currently recommends combinations according to treatment guidelines. WHO recognizes that not all of the fixed dose combinations (FDCs) in the WHO treatment guidelines exist, and encourages their development and rigorous testing. WHO also encourages development and testing of rectal dosage formulations. | |
| amodiaquine* | Tablet: 153 mg or 200 mg (as hydrochloride).
* To be used in combination with artesunate 50 mg. |
| artemether* | Oily injection: 80 mg/ mL in 1- mL ampoule.
* For use in the management of severe malaria. |
| artemether + lumefantrine* | Tablet: 20 mg + 120 mg.
Tablet (dispersible): 20 mg + 120 mg [c]. * Not recommended in the first trimester of pregnancy or in children below 5 kg. |
| artesunate* | Injection: ampoules, containing 60 mg anhydrous artesunic acid with a separate ampoule of 5% sodium bicarbonate solution.
For use in the management of severe malaria. Rectal dosage form: 50 mg [c]; 100 mg [c]; 200 mg capsules (for pre-referral treatment of severe malaria only; patients should be taken to an appropriate health facility for follow-up care) [c]. Tablet: 50 mg. * To be used in combination with either amodiaquine, mefloquine or sulfadoxine + pyrimethamine. |
| artesunate + amodiaquine* | Tablet: 25 mg + 67.5 mg; 50 mg + 135 mg; 100 mg + 270 mg.
* Other combinations that deliver the target doses required such as 153 mg or 200 mg (as hydrochloride) with 50 mg artesunate can be alternatives. |
| artesunate + mefloquine | Tablet: 25 mg + 55 mg; 100 mg + 220 mg. |
| artesunate + pyronaridine tetraphosphate a | Tablet: 60 mg + 180 mg
Granules: 20 mg + 60 mg [c]. a > 5 kg |
| chloroquine* | Oral liquid: 50 mg (as phosphate or sulfate)/5 mL.
Tablet: 100 mg; 150 mg (as phosphate or sulfate). * For use only for the treatment of P.vivax infection. |
| dihydroartemisinin + piperaquine phosphate
a |
Tablet: 20 mg + 160 mg; 40 mg + 320 mg
a > 5 kg |
| doxycycline* | Capsule: 100 mg (as hydrochloride or hyclate).
Tablet (dispersible): 100 mg (as monohydrate). * For use only in combination with quinine. |
| mefloquine* | Tablet: 250 mg (as hydrochloride).
* To be used in combination with artesunate 50 mg. |
| primaquine* | Tablet: 7.5 mg; 15 mg (as diphosphate).
* Only for use to achieve radical cure of P.vivax and P.ovale infections, given for 14 days. |
| quinine* | Injection: 300 mg quinine hydrochloride/ mL in 2- mL ampoule.
Tablet: 300 mg (quinine sulfate) or 300 mg (quinine bisulfate). * For use only in the management of severe malaria, and should be used in combination with doxycycline. |
| sulfadoxine + pyrimethamine* | Tablet: 500 mg + 25 mg.
* Only in combination with artesunate 50 mg. |
| 6.5.3.2 For prophylaxis | |
| chloroquine* | Oral liquid: 50 mg (as phosphate or sulfate)/5 mL.
Tablet: 150 mg (as phosphate or sulfate). * For use only in central American regions, for P.vivax infections. |
| doxycycline a | Solid oral dosage form: 100 mg (as hydrochloride or hyclate).
a >8 years. |
| mefloquine a | Tablet: 250 mg (as hydrochloride).
a >5 kg or >3 months. |
| proguanil* | Tablet: 100 mg (as hydrochloride).
* For use only in combination with chloroquine. |
| 6.5.4 Antipneumocystosis and antitoxoplasmosis medicines | |
| pyrimethamine | Tablet: 25 mg. |
| sulfadiazine | Tablet: 500 mg. |
| sulfamethoxazole + trimethoprim | Injection:
80 mg + 16 mg/ mL in 5- mL ampoule; 80 mg + 16 mg/ mL in 10- mL ampoule. Oral liquid: 200 mg + 40 mg/5 mL [c]. Tablet: 100 mg + 20 mg; 400 mg + 80 mg [c]. |
| Complementary List | |
| pentamidine | Tablet: 200 mg; 300 mg (as isethionate). |
| 6.5.5 Antitrypanosomal medicines | |
| 6.5.5.1 African trypanosomiasis | |
| Medicines for the treatment of 1st stage African trypanosomiasis | |
| pentamidine* | Powder for injection: 200 mg (as isetionate) in vial.
* To be used for the treatment of Trypanosoma brucei gambiense infection. |
| suramin sodium* | Powder for injection: 1 g in vial.
* To be used for the treatment of the initial phase of Trypanosoma brucei rhodesiense infection. |
| Medicines for the treatment of 2nd stage African trypanosomiasis | |
| eflornithine* | Injection: 200 mg (hydrochloride)/ mL in 100- mL bottle.
* To be used for the treatment of Trypanosoma brucei gambiense infection. |
| melarsoprol | Injection: 3.6% solution, 5- mL ampoule (180 mg of active
compound). |
| nifurtimox* | Tablet: 120 mg.
* Only to be used in combination with eflornithine, for the treatment of Trypanosoma brucei gambiense infection. |
| Complementary List [c] | |
| melarsoprol | Injection: 3.6% solution in 5- mL ampoule (180 mg of active compound). |
| 6.5.5.2 American trypanosomiasis | |
| benznidazole | Tablet: 12.5 mg [c];100 mg.
Tablet (scored): 50 mg. |
| nifurtimox | Tablet: 30 mg; 120 mg; 250 mg. |
| 7. ANTIMIGRAINE MEDICINES | |
| 7.1 For treatment of acute attack | |
| acetylsalicylic acid | Tablet: 300 mg to 500 mg. |
| ibuprofen [c] | Tablet: 200 mg; 400 mg. |
| paracetamol | Oral liquid: 120 mg/5 mL [c]; 125 mg/5 mL [c].
Tablet: 300 mg to 500 mg. |
| 7.2 For prophylaxis | |
| o propranolol | Tablet: 20 mg; 40 mg (hydrochloride). |
| 8. ANTINEOPLASTICS AND IMMUNOSUPPRESSIVES
Medicines listed below should be used according to protocols for treatment of the diseases. |
|
| 8.1 Immunosuppressive medicines | |
| Complementary List | |
| azathioprine | Powder for injection: 100 mg (as sodium salt) in vial.
Tablet (scored): 50 mg. |
| ciclosporin | Capsule: 25 mg.
Concentrate for injection: 50 mg/ mL in 1- mL ampoule for organ transplantation. |
| 8.2 Cytotoxic and adjuvant medicines | |
| Complementary List | |
| all-trans retinoid acid (ATRA) | Capsule: 10 mg.
– Acute promyelocytic leukaemia. |
| allopurinol [c] | Tablet: 100 mg; 300 mg. |
| asparaginase | Powder for injection: 10 000 IU in vial.
– Acute lymphoblastic leukaemia. |
| bendamustine | Injection: 45 mg/0.5 mL; 180 mg/2 mL.
– Chronic lymphocytic leukaemia – Follicular lymphoma |
| bleomycin | Powder for injection: 15 mg (as sulfate) in vial.
– Hodgkin lymphoma – Kaposi sarcoma – Ovarian germ cell tumour – Testicular germ cell tumour |
| calcium folinate | Injection: 3 mg/ mL in 10- mL ampoule.
Tablet: 15 mg. – Early stage colon cancer – Early stage rectal cancer – Gestational trophoblastic neoplasia – Metastatic colorectal cancer – Osteosarcoma – Burkitt lymphoma |
| capecitabine | Tablet: 150 mg; 500 mg.
– Early stage colon cancer – Early stage rectal cancer – Metastatic breast cancer – Metastatic colorectal cancer |
| carboplatin | Injection: 50 mg/5 mL; 150 mg/15 mL; 450 mg/45 mL; 600 mg/60 mL.
– Early stage breast cancer – Epithelial ovarian cancer – Nasopharyngeal cancer – Non-small cell lung cancer – Osteosarcoma – Retinoblastoma |
| chlorambucil | Tablet: 2 mg.
– Chronic lymphocytic leukaemia. |
| cisplatin | Injection: 50 mg/50 mL; 100 mg/100 mL.
– Cervical cancer (as a radio-sensitizer) – Head and neck cancer (as a radio-sensitizer) – Nasopharyngeal cancer (as a radio-sensitizer) – Non-small cell lung cancer – Osteosarcoma – Ovarian germ cell tumour – Testicular germ cell tumour |
| cyclophosphamide | Powder for injection: 500 mg in vial.
Tablet: 25 mg. – Chronic lymphocytic leukaemia – Diffuse large B-cell lymphoma – Early stage breast cancer – Gestational trophoblastic neoplasia – Hodgkin lymphoma – Follicular lymphoma – Rhabdomyosarcoma – Ewing sarcoma – Acute lymphoblastic leukaemia – Burkitt lymphoma – Metastatic breast cancer. |
| cytarabine | Powder for injection: 100 mg in vial.
– Acute myelogenous leukaemia – Acute lymphoblastic leukaemia – Acute promyelocytic leukaemia – Burkitt lymphoma. |
| dacarbazine | Powder for injection: 100 mg in vial.
– Hodgkin lymphoma |
| dactinomycin | Powder for injection: 500 micrograms in vial.
– Gestational trophoblastic neoplasia – Rhabdomyosarcoma – Wilms tumour |
| dasatinib | Tablet: 20 mg; 50 mg; 70 mg; 80 mg; 100 mg; 140 mg.
– Imatinib-resistant chronic myeloid leukaemia |
| daunorubicin | Powder for injection: 50 mg (hydrochloride) in vial.
– Acute lymphoblastic leukaemia – Acute myelogenous leukaemia – Acute promyelocytic leukaemia |
| docetaxel | Injection: 20 mg/ mL; 40 mg/ mL.
– Early stage breast cancer – Metastatic breast cancer – Metastatic prostate cancer |
| doxorubicin | Powder for injection: 10 mg; 50 mg (hydrochloride) in vial.
– Diffuse large B-cell lymphoma – Early stage breast cancer – Hodgkin lymphoma – Kaposi sarcoma – Follicular lymphoma – Metastatic breast cancer – Osteosarcoma – Ewing sarcoma – Acute lymphoblastic leukaemia – Wilms tumour – Burkitt lymphoma |
| etoposide | Capsule: 100 mg.
Injection: 20 mg/ mL in 5- mL ampoule. – Testicular germ cell tumour – Gestational trophoblastic neoplasia – Hodgkin lymphoma – Non-small cell lung cancer – Ovarian germ cell tumour – Retinoblastoma – Ewing sarcoma – Acute lymphoblastic leukaemia – Burkitt lymphoma |
| filgrastim | Injection: 120 micrograms/0.2 mL; 300 micrograms/0.5 mL; 480 micrograms/0.8 mL in pre-filled syringe 300 micrograms/mL in 1- mL vial, 480 mg/1.6 mL in 1.6- mL vial.
– Primary prophylaxis in patients at high risk for developing febrile neutropenia associated with myelotoxic chemotherapy. – Secondary prophylaxis for patients who have experienced neutropenia following prior myelotoxic chemotherapy – To facilitate administration of dose dense chemotherapy regimens |
| fludarabine | Powder for injection: 50 mg (phosphate) in vial.
Tablet: 10 mg – Chronic lymphocytic leukaemia. |
| fluorouracil | Injection: 50 mg/ mL in 5- mL ampoule.
– Early stage breast cancer – Early stage colon cancer – Early stage rectal cancer – Metastatic colorectal cancer – Nasopharyngeal cancer. |
| gemcitabine | Powder for injection: 200 mg in vial, 1 g in vial.
– Epithelial ovarian cancer – Non-small cell lung cancer |
| hydroxycarbamide | Solid oral dosage form: 200 mg; 250 mg; 300 mg; 400 mg; 500 mg;
1 g. – Chronic myeloid leukaemia. |
| ifosfamide | Powder for injection: 500 mg vial; 1-g vial; 2-g vial.
– Testicular germ cell tumour – Ovarian germ cell tumour – Osteosarcoma – Rhabdomyosarcoma – Ewing sarcoma |
| imatinib | Tablet: 100 mg; 400 mg.
– Chronic myeloid leukaemia – Gastrointestinal stromal tumour |
| irinotecan | Injection: 40 mg/2 mL in 2- mL vial; 100 mg/5 mL in 5- mL vial; 500 mg/25 mL in 25- mL vial.
– Metastatic colorectal cancer. |
| mercaptopurine | Tablet: 50 mg.
– Acute lymphoblastic leukaemia – Acute promyelocytic leukaemia. |
| mesna | Injection: 100 mg/ mL in 4- mL and 10- mL ampoules.
Tablet: 400 mg; 600 mg. – Testicular germ cell tumour – Ovarian germ cell tumour – Osteosarcoma – Rhabdomyosarcoma – Ewing sarcoma. |
| methotrexate | Powder for injection: 50 mg (as sodium salt) in vial.
Tablet: 2.5 mg (as sodium salt). – Early stage breast cancer – Gestational trophoblastic neoplasia – Osteosarcoma – Acute lymphoblastic leukaemia – Acute promyelocytic leukaemia |
| nilotinib | Capsule: 150 mg; 200 mg.
– Imatinib-resistant chronic myeloid leukaemia |
| oxaliplatin | Injection: 50 mg/10 mL in 10- mL vial; 100 mg/20 mL in 20- mL vial; 200 mg/40 mL in 40- mL vial.
Powder for injection: 50 mg, 100 mg in vial. – Early stage colon cancer – Metastatic colorectal cancer |
| paclitaxel | Powder for injection: 6 mg/ mL.
– Epithelial ovarian cancer – Early stage breast cancer – Metastatic breast cancer – Kaposi sarcoma – Nasopharyngeal cancer – Non-small cell lung cancer – Ovarian germ cell tumour |
| procarbazine | Capsule: 50 mg (as hydrochloride). |
| rituximab | Injection: 100 mg/10 mL in 10- mL vial; 500 mg/50 mL in 50- mL vial.
– Diffuse large B-cell lymphoma – Chronic lymphocytic leukaemia – Follicular lymphoma. |
| tioguanine [c] | Solid oral dosage form: 40 mg.
– Acute lymphoblastic leukaemia. |
| trastuzumab | Powder for injection: 60 mg; 150 mg; 440 mg in vial
– Early stage HER2 positive breast cancer – Metastatic HER2 positive breast cancer. |
| vinblastine | Powder for injection: 10 mg (sulfate) in vial.
– Hodgkin lymphoma – Kaposi sarcoma. – Testicular germ cell tumour – Ovarian germ cell tumour |
| vincristine | Powder for injection: 1 mg; 5 mg (sulfate) in vial.
– Diffuse large B-cell lymphoma – Gestational trophoblastic neoplasia – Hodgkin lymphoma – Kaposi sarcoma – Follicular lymphoma – Retinoblastoma – Rhabdomyosarcoma – Ewing sarcoma – Acute lymphoblastic leukaemia – Wilms tumour – Burkitt lymphoma. |
| vinorelbine | Injection: 10 mg/mL in 1- mL vial; 50 mg/5 mL in 5- mL vial.
– Non-small cell lung cancer – Metastatic breast cancer |
| zoledronic acid | Concentrate solution for infusion: 4 mg/5 mL in 5- mL vial.
Solution for infusion: 4 mg/100 mL in 100- mL bottle. – Malignancy-related bone disease |
| 8.3 Hormones and antihormones | |
| Complementary List | |
| o anastrozole | Tablet: 1 mg.
– Early stage breast cancer – Metastatic breast cancer. |
| o bicalutamide | Tablet: 50 mg.
– Metastatic prostate cancer. |
| dexamethasone | Injection: 4 mg/ mL in 1- mL ampoule (as disodium phosphate salt).
Oral liquid: 2 mg/5 mL [c]. – Acute lymphoblastic leukaemia. |
| o leuprorelin | Dose form
– Early stage breast cancer – Metastatic prostate cancer |
| hydrocortisone | Powder for injection: 100 mg (as sodium succinate) in vial.
– Acute lymphoblastic leukaemia. |
| methylprednisolone [c] | Injection: 40 mg/ mL (as sodium succinate) in 1- mL single-dose vial and
5- mL multi-dose vials; 80 mg/ mL (as sodium succinate) in 1- mL single-dose vial. – Acute lymphoblastic leukamia. |
| o prednisolone | Oral liquid: 5 mg/ mL [c].
Tablet: 5 mg; 25 mg. – Chronic lymphocytic leukaemia – Diffuse large B-cell lymphoma – Hodgkin lymphoma – Follicular lymphoma – Acute lymphoblastic leukaemia – Burkitt lymphoma |
| tamoxifen | Tablet: 10 mg; 20 mg (as citrate).
– Early stage breast cancer – Metastatic breast cancer |
| 9. ANTIPARKINSONISM MEDICINES | |
| o biperiden | Injection: 5 mg (lactate) in 1- mL ampoule.
Tablet: 2 mg (hydrochloride). |
| levodopa + o carbidopa | Tablet: 100 mg + 10 mg; 100 mg + 25 mg; 250 mg + 25 mg |
| 10. MEDICINES AFFECTING THE BLOOD | |
| 10.1 Antianaemia medicines | |
| ferrous salt | Oral liquid: equivalent to 25 mg iron (as sulfate)/ mL.
Tablet: equivalent to 60 mg iron. |
| ferrous salt + folic acid | Tablet: equivalent to 60 mg iron + 400 micrograms folic acid (nutritional supplement for use during pregnancy). |
| folic acid | Tablet: 400 micrograms*; 1 mg; 5 mg.
*periconceptual use for prevention of first occurrence of neural tube defects |
| hydroxocobalamin | Injection: 1 mg (as acetate, as hydrochloride or as sulfate) in 1- mL ampoule. |
| Complementary List | |
| o erythropoiesis-stimulating agents* | Injection: pre-filled syringe
1000IU/ 0.5 mL; 2000IU/ 0.5 mL; 3000IU/ 0.3 mL; 4000IU/ 0.4 mL; 5000IU/ 0.5 mL; 6000IU/ 0.6 mL; 8000IU/ 0.8mL; 10 000IU/ 1 mL; 20 000IU/ 0.5 mL; 40 000IU/ 1 mL * the square box applies to epoetin alfa, beta and theta, darbepoetin alfa, methoxy polyethylene glycol-epoetin beta,and their respective biosimilars. |
| 10.2 Medicines affecting coagulation | |
| o enoxaparin* | Injection: ampoule or pre-filled syringe
20 mg/0.2 mL; 40 mg/0.4 mL; 60 mg/0.6 mL; 80 mg/0.8 mL; 100 mg/1 mL; 120 mg/0.8 mL; 150 mg/1 mL *Alternatives are limited to nadroparin and dalteparin |
| heparin sodium | Injection: 1000 IU/ mL; 5000 IU/ mL; 20 000 IU/ mL in 1- mL ampoule. |
| phytomenadione | Injection: 1 mg/ mL [c]; 10 mg/ mL in 5- mL ampoule.
Tablet: 10 mg. |
| protamine sulfate | Injection: 10 mg/ mL in 5- mL ampoule. |
| tranexamic acid | Injection: 100 mg/ mL in 10- mL ampoule. |
| o warfarin | Tablet: 1 mg; 2 mg; 5 mg (sodium salt). |
| Complementary List [c] | |
| desmopressin | Injection: 4 micrograms/ mL (as acetate) in 1- mL ampoule.
Nasal spray: 10 micrograms (as acetate) per dose |
| heparin sodium | Injection: 1000 IU/ mL; 5000 IU/ mL in 1- mL ampoule. |
| protamine sulfate | Injection: 10 mg/ mL in 5- mL ampoule. |
| o warfarin | Tablet: 0.5 mg; 1 mg; 2 mg; 5 mg (sodium salt). |
| 10.3 Other medicines for haemoglobinopathies | |
| Complementary List | |
| deferoxamine* | Powder for injection: 500 mg (mesilate) in vial.
* Deferasirox oral form may be an alternative, depending on cost and availability. |
| hydroxycarbamide | Solid oral dosage form: 200 mg; 500 mg; 1 g. |
| 11. BLOOD PRODUCTS OF HUMAN ORIGIN AND PLASMA SUBSTITUTES | |
| 11.1 Blood and blood components | |
| In accordance with the World Health Assembly resolution WHA63.12, WHO recognizes that achieving self- sufficiency, unless special circumstances preclude it, in the supply of safe blood components based on voluntary, non-remunerated blood donation, and the security of that supply are important national goals to prevent blood shortages and meet the transfusion requirements of the patient population. All preparations should comply with the WHO requirements. | |
| fresh–frozen plasma | |
| platelets | |
| red blood cells | |
| whole blood | |
| 11.2 Plasma-derived medicines | |
| All human plasma-derived medicines should comply with the WHO requirements. | |
| 11.2.1 Human immunoglobulins | |
| anti-D immunoglobulin | Injection: 250 micrograms in single-dose vial. |
| Anti-rabies immunoglobulin | Injection: 150 IU/ mL in vial. |
| Anti-tetanus immunoglobulin | Injection: 500 IU in vial. |
| Complementary List | |
| normal immunoglobulin | Intramuscular administration: 16% protein solution.*
Intravenous administration: 5%; 10% protein solution.** Subcutaneous administration: 15%; 16% protein solution.* * Indicated for primary immune deficiency. **Indicated for primary immune deficiency and Kawasaki disease. |
| 11.2.2 Blood coagulation factors | |
| Complementary List | |
| o coagulation factor VIII | Powder for injection: 500 IU/vial. |
| o coagulation factor IX | Powder for injection: 500 IU/vial, 1000 IU/vial. |
| 11.3 Plasma substitutes | |
| o dextran 70* | Injectable solution: 6%.
* Polygeline, injectable solution, 3.5% is considered as equivalent. |
| 12. CARDIOVASCULAR MEDICINES
Fixed-dose combinations for non-communicable diseases may have advantages over the single medicines given concomitantly, including increased adherence and reduced pill burden. The potential value of fixed-dose combinations of currently listed essential medicines, with regulatory approval and demonstrated bioavailability for the management of chronic non-communicable diseases, is recognized. |
|
| 12.1 Antianginal medicines | |
| o bisoprolol* | Tablet: 1.25 mg; 5 mg.
* o includes metoprolol and carvedilol as alternatives. |
| glyceryl trinitrate | Tablet (sublingual): 500 micrograms. |
| o isosorbide dinitrate | Tablet (sublingual): 5 mg. |
| verapamil | Tablet: 40 mg; 80 mg (hydrochloride). |
| 12.2 Antiarrhythmic medicines | |
| o bisoprolol* | Tablet: 1.25 mg; 5 mg.
* o includes metoprolol and carvedilol as alternatives. |
| digoxin | Injection: 250 micrograms/ mL in 2- mL ampoule.
Oral liquid: 50 micrograms/ mL. Tablet: 62.5 micrograms; 250 micrograms. |
| epinephrine (adrenaline) | Injection: 100 micrograms/ mL (as acid tartrate or
hydrochloride) in 10- mL ampoule. |
| lidocaine | Injection: 20 mg (hydrochloride)/ mL in 5- mL ampoule. |
| verapamil | Injection: 2.5 mg (hydrochloride)/ mL in 2- mL ampoule.
Tablet: 40 mg; 80 mg (hydrochloride). |
| Complementary List | |
| amiodarone | Injection: 50 mg/ mL in 3- mL ampoule (hydrochloride).
Tablet: 100 mg; 200 mg; 400 mg (hydrochloride). |
| 12.3 Antihypertensive medicines | |
| o amlodipine | Tablet: 5 mg (as maleate, mesylate or besylate). |
| o bisoprolol* | Tablet: 1.25 mg; 5 mg.
* includes atenolol, metoprolol and carvedilol as alternatives. Atenolol should not be used as a first-line agent in uncomplicated hypertension in patients >60 years |
| o enalapril | Tablet: 2.5 mg; 5 mg (as hydrogen maleate). |
| hydralazine* | Powder for injection: 20 mg (hydrochloride) in ampoule.
Tablet: 25 mg; 50 mg (hydrochloride). * Hydralazine is listed for use only in the acute management of severe pregnancy-induced hypertension. Its use in the treatment of essential hypertension is not recommended in view of the evidence of greater efficacy and safety of other medicines. |
| o hydrochlorothiazide | Oral liquid: 50 mg/5 mL.
Solid oral dosage form: 12.5 mg; 25 mg. |
| methyldopa* | Tablet: 250 mg.
* Methyldopa is listed for use only in the management of pregnancy-induced hypertension. Its use in the treatment of essential hypertension is not recommended in view of the evidence of greater efficacy and safety of other medicines. |
| o losartan | Tablet: 25 mg; 50 mg; 100 mg. |
| Complementary List | |
| sodium nitroprusside | Powder for infusion: 50 mg in ampoule. |
| 12.4 Medicines used in heart failure | |
| o bisoprolol* | Tablet: 1.25 mg; 5 mg.
*o includes metoprolol and carvedilol as alternatives. |
| digoxin | Injection: 250 micrograms/ mL in 2- mL ampoule.
Oral liquid: 50 micrograms/ mL. Tablet: 62.5 micrograms; 250 micrograms. |
| o enalapril | Tablet: 2.5 mg; 5 mg (as hydrogen maleate). |
| o furosemide | Injection: 10 mg/ mL in 2- mL ampoule.
Oral liquid: 20 mg/5 mL [c]. Tablet: 40 mg. |
| o hydrochlorothiazide | Oral liquid: 50 mg/5 mL.
Solid oral dosage form: 25 mg. |
| o losartan | Tablet: 25 mg; 50 mg; 100 mg |
| spironolactone | Tablet: 25 mg. |
| Complementary List | |
| dopamine | Injection: 40 mg/ mL (hydrochloride) in 5- mL vial. |
| 12.5 Antithrombotic medicines | |
| 12.5.1 Anti-platelet medicines | |
| acetylsalicylic acid | Tablet: 100 mg. |
| clopidogrel | Tablet: 75 mg; 300 mg |
| 12.5.2 Thrombolytic medicines | |
| Complementary List | |
| streptokinase | Powder for injection: 1.5 million IU in vial. |
| 12.6 Lipid-lowering agents | |
| o simvastatin* | Tablet: 5 mg; 10 mg; 20 mg; 40 mg.
* For use in high-risk patients. |
| 13. DERMATOLOGICAL MEDICINES (topical) | |
| 13.1 Antifungal medicines | |
| o miconazole | Cream or ointment: 2% (nitrate). |
| selenium sulfide | Detergent–based suspension: 2%. |
| sodium thiosulfate | Solution: 15%. |
| terbinafine | Cream: 1% or Ointment: 1% terbinafine hydrochloride. |
| 13.2 Anti-infective medicines | |
| mupirocin | Cream (as mupirocin calcium): 2%.
Ointment: 2%. |
| potassium permanganate | Aqueous solution: 1:10 000. |
| silver sulfadiazine a | Cream: 1%.
a >2 months. |
| 13.3 Anti-inflammatory and antipruritic medicines | |
| o betamethasone a | Cream or ointment: 0.1% (as valerate).
a Hydrocortisone preferred in neonates. |
| o calamine | Lotion. |
| o hydrocortisone | Cream or ointment: 1% (acetate). |
| 13.4 Medicines affecting skin differentiation and proliferation | |
| benzoyl peroxide | Cream or lotion: 5%. |
| coal tar | Solution: 5%. |
| fluorouracil | Ointment: 5%. |
| o podophyllum resin | Solution: 10% to 25%. |
| salicylic acid | Solution: 5%. |
| urea | Cream or ointment: 5%; 10%. |
| 13.5 Scabicides and pediculicides | |
| o benzyl benzoate a | Lotion: 25%.
a >2 years. |
| permethrin | Cream: 5%.
Lotion: 1%. |
| 14. DIAGNOSTIC AGENTS | |
| 14.1 Ophthalmic medicines | |
| fluorescein | Eye drops: 1% (sodium salt). |
| o tropicamide | Eye drops: 0.5%. |
| 14.2 Radiocontrast media | |
| o amidotrizoate | Injection: 140 mg to 420 mg iodine (as sodium or meglumine salt)/ mL in 20- mL ampoule. |
| barium sulfate | Aqueous suspension. |
| o iohexol | Injection: 140 mg to 350 mg iodine/ mL in 5- mL; 10- mL; 20- mL ampoules. |
| Complementary List | |
| barium sulfate [c] | Aqueous suspension. |
| o meglumine iotroxate | Solution: 5 g to 8 g iodine in 100 mL to 250 mL. |
| 15. DISINFECTANTS AND ANTISEPTICS | |
| 15.1 Antiseptics | |
| o chlorhexidine | Solution: 5% (digluconate). |
| o ethanol | Solution: 70% (denatured). |
| o povidone iodine | Solution: 10% (equivalent to 1% available iodine). |
| 15.2 Disinfectants | |
| alcohol based hand rub | Solution: containing ethanol 80% volume /volume
Solution: containing isopropyl alcohol 75% volume/volume |
| o chlorine base compound | Powder: (0.1% available chlorine) for solution. |
| o chloroxylenol | Solution: 4.8%. |
| glutaral | Solution: 2%. |
| 16. DIURETICS | |
| amiloride | Tablet: 5 mg (hydrochloride). |
| o furosemide | Injection: 10 mg/ mL in 2- mL ampoule.
Oral liquid: 20 mg/5 mL [c]. Tablet: 10 mg [c]; 20 mg [c]; 40 mg. |
| o hydrochlorothiazide | Solid oral dosage form: 25 mg. |
| mannitol | Injectable solution: 10%; 20%. |
| spironolactone | Tablet: 25 mg. |
| Complementary List [c] | |
| o hydrochlorothiazide | Tablet (scored): 25 mg. |
| mannitol | Injectable solution: 10%; 20%. |
| spironolactone | Oral liquid: 5 mg/5 mL; 10 mg/5 mL; 25 mg/5 mL.
Tablet: 25 mg. |
| 17. GASTROINTESTINAL MEDICINES | |
| Complementary List [c] | |
| o pancreatic enzymes | Age-appropriate formulations and doses including lipase, protease and amylase. |
| 17.1 Antiulcer medicines | |
| o omeprazole | Powder for injection: 40 mg in vial
Powder for oral liquid: 20 mg; 40 mg sachets. Solid oral dosage form: 10 mg; 20 mg; 40 mg. |
| o ranitidine | Injection: 25 mg/ mL (as hydrochloride) in 2- mL ampoule.
Oral liquid: 75 mg/5 mL (as hydrochloride). Tablet: 150 mg (as hydrochloride). |
| 17.2 Antiemetic medicines | |
| dexamethasone | Injection: 4 mg/ mL in 1- mL ampoule (as disodium phosphate salt).
Oral liquid: 0.5 mg/5 mL; 2 mg/5 mL. Solid oral dosage form: 0.5 mg; 0.75 mg; 1.5 mg; 4 mg. |
| metoclopramide a | Injection: 5 mg (hydrochloride)/ mL in 2- mL ampoule.
Oral liquid: 5 mg/5 mL [c]. Tablet: 10 mg (hydrochloride). a Not in neonates. |
| ondansetron a | Injection: 2 mg base/ mL in 2- mL ampoule (as hydrochloride).
Oral liquid: 4 mg base/5 mL. Solid oral dosage form: Eq 4 mg base; Eq 8 mg base; Eq 24 mg base. a >1 month. |
| 17.3 Anti-inflammatory medicines | |
| o sulfasalazine | Retention enema. Suppository: 500 mg.
Tablet: 500 mg. |
| Complementary List | |
| o hydrocortisone | Retention enema.
Suppository: 25 mg (acetate). (the o only applies to hydrocortisone retention enema). |
| 17.4 Laxatives | |
| o senna | Tablet: 7.5 mg (sennosides) (or traditional dosage forms). |
| 17.5 Medicines used in diarrhoea | |
| 17.5.1 Oral rehydration | |
| oral rehydration salts | Powder for dilution in 200 mL; 500 mL; 1 L.
glucose: 75 mEq sodium: 75 mEq or mmol/L chloride: 65 mEq or mmol/L potassium: 20 mEq or mmol/L citrate: 10 mmol/L osmolarity: 245 mOsm/L glucose: 13.5 g/L sodium chloride: 2.6 g/L potassium chloride: 1.5 g/L trisodium citrate dihydrate*: 2.9 g/L *trisodium citrate dihydrate may be replaced by sodium hydrogen carbonate (sodium bicarbonate) 2.5 g/L. However, as the stability of this latter formulation is very poor under tropical conditions, it is recommended only when manufactured for immediate use. |
| 17.5.2 Medicines for diarrhoea | |
| zinc sulfate* | Solid oral dosage form: 20 mg.
* In acute diarrhoea zinc sulfate should be used as an adjunct to oral rehydration salts. |
| 18. HORMONES, OTHER ENDOCRINE MEDICINES AND CONTRACEPTIVES | |
| 18.1 Adrenal hormones and synthetic substitutes | |
| fludrocortisone | Tablet: 100 micrograms (acetate). |
| hydrocortisone | Tablet: 5 mg; 10 mg; 20 mg. |
| 18.2 Androgens | |
| Complementary List | |
| testosterone | Injection: 200 mg (enanthate) in 1- mL ampoule. |
| 18.3 Contraceptives | |
| 18.3.1 Oral hormonal contraceptives | |
| o ethinylestradiol + o levonorgestrel | Tablet: 30 micrograms + 150 micrograms. |
| o ethinylestradiol + o norethisterone | Tablet: 35 micrograms + 1 mg. |
| levonorgestrel | Tablet: 30 micrograms; 750 micrograms (pack of two); 1.5 mg. |
| ulipristal | Tablet: 30 mg (as acetate) |
| 18.3.2 Injectable hormonal contraceptives | |
| estradiol cypionate + medroxyprogesterone acetate | Injection: 5 mg + 25 mg. |
| medroxyprogesterone acetate | Injection (intramuscular): 150 mg/ mL in 1- mL vial.
Injection (subcutaneous): 104 mg/0.65 mL in pre-filled syringe or single-dose injection delivery system. |
| norethisterone enantate | Oily solution: 200 mg/ mL in 1- mL ampoule. |
| 18.3.3 Intrauterine devices | |
| copper-containing device | |
| levonorgestrel-releasing intrauterine system | Intrauterine system with reservoir containing 52 mg of levonorestrel |
| 18.3.4 Barrier methods | |
| condoms | |
| diaphragms | |
| 18.3.5 Implantable contraceptives | |
| etonogestrel-releasing implant | Single-rod etonogestrel-releasing implant, containing 68 mg of etonogestrel. |
| levonorgestrel-releasing implant | Two-rod levonorgestrel-releasing implant, each rod containing 75 mg of levonorgestrel (150 mg total). |
| 18.3.6 Intravaginal contraceptives | |
| progesterone vaginal ring* | Progesterone-releasing vaginal ring containing 2.074 g of micronized progesterone.
*For use in women actively breastfeeding at least 4 times per day |
| 18.4 Estrogens | |
| 18.5 Insulins and other medicines used for diabetes | |
| o gliclazide* | Solid oral dosage form: (controlled-release tablets) 30 mg; 60 mg;
80 mg. * glibenclamide not suitable above 60 years. |
| glucagon | Injection: 1 mg/ mL. |
| insulin injection (soluble) | Injection: 40 IU/ mL in 10- mL vial; 100 IU/ mL in 10- mL vial. |
| intermediate-acting insulin | Injection: 40 IU/ mL in 10- mL vial; 100 IU/ mL in 10- mL vial (as compound insulin zinc suspension or isophane insulin). |
| metformin | Tablet: 500 mg (hydrochloride). |
| Complementary List [c] | |
| metformin | Tablet: 500 mg (hydrochloride). |
| 18.6 Ovulation inducers | |
| Complementary List | |
| clomifene | Tablet: 50 mg (citrate). |
| 18.7 Progestogens | |
| o medroxyprogesterone acetate | Tablet: 5 mg. |
| 18.8 Thyroid hormones and antithyroid medicines | |
| levothyroxine | Tablet: 25 micrograms [c]; 50 micrograms; 100 micrograms (sodium salt). |
| potassium iodide | Tablet: 60 mg. |
| o propylthiouracil | Tablet: 50 mg. |
| Complementary List [c] | |
| Lugol’s solution | Oral liquid: about 130 mg total iodine/ mL. |
| potassium iodide | Tablet: 60 mg. |
| propylthiouracil | Tablet: 50 mg. |
| 19. IMMUNOLOGICALS | |
| 19.1 Diagnostic agents | |
| All tuberculins should comply with the WHO requirements for tuberculins. | |
| tuberculin, purified protein derivative (PPD) | Injection. |
| 19.2 Sera and immunoglobulins | |
| All plasma fractions should comply with the WHO requirements. | |
| Anti-venom immunoglobulin* | Injection.
* Exact type to be defined locally. |
| diphtheria antitoxin | Injection: 10 000 IU; 20 000 IU in vial. |
| 19.3 Vaccines | |
| WHO immunization policy recommendations are published in vaccine position papers on the basis of recommendations made by the Strategic Advisory Group of Experts on Immunization (SAGE).
WHO vaccine position papers are updated three to four times per year. The list below details the vaccines for which there is a recommendation from SAGE and a corresponding WHO position paper as at 10 February 2017. The most recent versions of the WHO position papers, reflecting the current evidence related to a specific vaccine and the related recommendations, can be accessed at any time on the WHO website at: https://www.who.int/immunization/documents/positionpapers/en/index.html. Vaccine recommendations may be universal or conditional (e.g., in certain regions, in some high-risk populations or as part of immunization programmes with certain characteristics). Details are available in the relevant position papers, and in the Summary Tables of WHO Routine Immunization Recommendations available on the WHO website at: https://www.who.int/immunization/policy/immunization_tables/en/index.html. Selection of vaccines from the Model List will need to be determined by each country after consideration of international recommendations, epidemiology and national priorities. All vaccines should comply with the WHO requirements for biological substances. WHO noted the need for vaccines used in children to be polyvalent. |
|
| Recommendations for all | |
| BCG vaccine | |
| diphtheria vaccine | |
| Haemophilus influenzae type b vaccine | |
| hepatitis B vaccine | |
| HPV vaccine | |
| measles vaccine | |
| pertussis vaccine | |
| pneumococcal vaccine | |
| poliomyelitis vaccine | |
| rotavirus vaccine | |
| rubella vaccine | |
| tetanus vaccine | |
| Recommendations for certain regions | |
| Japanese encephalitis vaccine | |
| yellow fever vaccine | |
| tick-borne encephalitis vaccine | |
| Recommendations for some high-risk populations | |
| cholera vaccine | |
| hepatitis A vaccine | |
| meningococcal meningitis vaccine | |
| rabies vaccine | |
| typhoid vaccine | |
| Recommendations for immunization programmes with certain characteristics | |
| influenza vaccine (seasonal) | |
| mumps vaccine | |
| varicella vaccine | |
| 20. MUSCLE RELAXANTS (PERIPHERALLY-ACTING) AND CHOLINESTERASE INHIBITORS | |
| o atracurium | Injection: 10 mg/ mL (besylate). |
| neostigmine | Injection: 500 micrograms in 1- mL ampoule; 2.5 mg (metilsulfate) in 1- mL ampoule.
Tablet: 15 mg (bromide). |
| suxamethonium | Injection: 50 mg (chloride)/ mL in 2- mL ampoule.
Powder for injection (chloride), in vial. |
| o vecuronium [c] | Powder for injection: 10 mg (bromide) in vial. |
| Complementary List | |
| pyridostigmine | Injection: 1 mg in 1- mL ampoule.
Tablet: 60 mg (bromide). |
| o vecuronium | Powder for injection: 10 mg (bromide) in vial. |
| 21. OPHTHALMOLOGICAL PREPARATIONS | |
| 21.1 Anti-infective agents | |
| aciclovir | Ointment: 3% W/W. |
| azithromycin | Solution (eye drops): 1.5%. |
| erythromycin* | Ointment: 0.5% [c]
*Infections due to Chlamydia trachomatis or Neisseria gonorrhoea. |
| o gentamicin | Solution (eye drops): 0.3% (sulfate). |
| natamycin | Suspension: (eye drops): 5% |
| o ofloxacin | Solution (eye drops): 0.3%. |
| o tetracycline | Eye ointment: 1% (hydrochloride). |
| 21.2 Anti-inflammatory agents | |
| o prednisolone | Solution (eye drops): 0.5% (sodium phosphate). |
| 21.3 Local anaesthetics | |
| o tetracaine a | Solution (eye drops): 0.5% (hydrochloride).
a Not in preterm neonates. |
| 21.4 Miotics and antiglaucoma medicines | |
| acetazolamide | Tablet: 250 mg. |
| latanoprost | Solution (eye drops): latanoprost 50 micrograms/mL |
| o pilocarpine | Solution (eye drops): 2%; 4% (hydrochloride or nitrate). |
| o timolol | Solution (eye drops): 0.25%; 0.5% (as hydrogen maleate). |
| 21.5 Mydriatics | |
| atropine* a | Solution (eye drops): 0.1%; 0.5%; 1% (sulfate).
* [c] Or homatropine (hydrobromide) or cyclopentolate (hydrochloride). a >3 months. |
| Complementary List | |
| epinephrine (adrenaline) | Solution (eye drops): 2% (as hydrochloride). |
| 21.6 Anti-vascular endothelial growth factor (VEGF) preparations | |
| Complementary List | |
| bevacizumab | Injection: 25 mg/ mL. |
| 22. OXYTOCICS AND ANTIOXYTOCICS | |
| 22.1 Oxytocics | |
| o ergometrine | Injection: 200 micrograms (hydrogen maleate) in 1- mL ampoule. |
| misoprostol | Tablet: 200 micrograms.
– Management of incomplete abortion and miscarriage; – Prevention and treatment of postpartum haemorrhage where oxytocin is not available or cannot be safely used Vaginal tablet: 25 micrograms.* * Only for use for induction of labour where appropriate facilities are available. |
| oxytocin | Injection: 10 IU in 1- mL. |
| Complementary List | |
| mifepristone* – misoprostol*
Where permitted under national law and where culturally acceptable. |
Tablet 200 mg – tablet 200 micrograms.
* Requires close medical supervision. |
| 22.2 Antioxytocics (tocolytics) | |
| nifedipine | Immediate-release capsule: 10 mg. |
| 23. PERITONEAL DIALYSIS SOLUTION | |
| Complementary List | |
| intraperitoneal dialysis solution (of appropriate composition) | Parenteral solution. |
| 24. MEDICINES FOR MENTAL AND BEHAVIOURAL DISORDERS | |
| 24.1 Medicines used in psychotic disorders | |
| o chlorpromazine | Injection: 25 mg (hydrochloride)/ mL in 2- mL ampoule.
Oral liquid: 25 mg (hydrochloride)/5 mL. Tablet: 100 mg (hydrochloride). |
| o fluphenazine | Injection: 25 mg (decanoate or enantate) in 1- mL ampoule. |
| o haloperidol | Injection: 5 mg in 1- mL ampoule.
Tablet: 2 mg; 5 mg. |
| risperidone | Solid oral dosage form: 0.25 mg to 6.0 mg. |
| Complementary List | |
| chlorpromazine [c] | Injection: 25 mg (hydrochloride)/ mL in 2- mL ampoule.
Oral liquid: 25 mg (hydrochloride)/5 mL. Tablet: 10 mg; 25 mg; 50 mg; 100 mg (hydrochloride). |
| clozapine | Solid oral dosage form: 25 to 200 mg. |
| haloperidol [c] | Injection: 5 mg in 1- mL ampoule.
Oral liquid: 2 mg/ mL. Solid oral dosage form: 0.5 mg; 2 mg; 5 mg. |
| 24.2 Medicines used in mood disorders | |
| 24.2.1 Medicines used in depressive disorders | |
| o amitriptyline | Tablet: 25 mg; 75mg. (hydrochloride). |
| fluoxetine | Solid oral dosage form: 20 mg (as hydrochloride). |
| Complementary List [c] | |
| fluoxetine a | Solid oral dosage form: 20 mg (as hydrochloride).
a >8 years. |
| 24.2.2 Medicines used in bipolar disorders | |
| carbamazepine | Tablet (scored): 100 mg; 200 mg. |
| lithium carbonate | Solid oral dosage form: 300 mg. |
| valproic acid (sodium valproate) | Tablet (enteric-coated): 200 mg; 500 mg (sodium valproate). |
| 24.3 Medicines for anxiety disorders | |
| o diazepam | Tablet (scored): 2 mg; 5 mg. |
| 24.4 Medicines used for obsessive compulsive disorders | |
| clomipramine | Capsule: 10 mg; 25 mg (hydrochloride). |
| 24.5 Medicines for disorders due to psychoactive substance use | |
| nicotine replacement therapy (NRT) | Chewing gum: 2 mg; 4 mg (as polacrilex).
Transdermal patch: 5 mg to 30 mg/16 hrs; 7 mg to 21 mg/24 hrs. |
| Complementary List | |
| o methadone* | Concentrate for oral liquid: 5 mg/ mL; 10 mg/ mL (hydrochloride).
Oral liquid: 5 mg/5 mL; 10 mg/5 mL (hydrochloride). * The square box is added to include buprenorphine. The medicines should only be used within an established support programme. |
| 25. MEDICINES ACTING ON THE RESPIRATORY TRACT | |
| 25.1 Antiasthmatic and medicines for chronic obstructive pulmonary disease | |
| o beclometasone | Inhalation (aerosol): 50 micrograms (dipropionate) per dose; 100 micrograms (dipropionate) per dose (as CFC free forms). |
| o budesonide [c] | Inhalation (aerosol): 100 micrograms per dose; 200 micrograms per dose. |
| o budesonide + formoterol | Dry powder inhaler: 100 micrograms + 6 micrograms per dose; 200 micrograms + 6 micrograms per dose |
| epinephrine (adrenaline) | Injection: 1 mg (as hydrochloride or hydrogen tartrate) in 1- mL ampoule. |
| ipratropium bromide | Inhalation (aerosol): 20 micrograms/metered dose. |
| o salbutamol | Inhalation (aerosol): 100 micrograms (as sulfate) per dose.
Injection: 50 micrograms (as sulfate)/ mL in 5- mL ampoule. Metered dose inhaler (aerosol): 100 micrograms (as sulfate) per dose. Respirator solution for use in nebulizers: 5 mg (as sulfate)/ mL. |
| 26. SOLUTIONS CORRECTING WATER, ELECTROLYTE AND ACID–BASE DISTURBANCES | |
| 26.1 Oral | |
| oral rehydration salts | See section 17.5.1. |
| potassium chloride | Powder for solution. |
| 26.2 Parenteral | |
| glucose | Injectable solution: 5% (isotonic); 10% (hypertonic);
50% (hypertonic). |
| glucose with sodium chloride | Injectable solution: 4% glucose, 0.18% sodium chloride (equivalent to Na+ 30 mmol/L, Cl- 30 mmol/L).
Injectable solution: 5% glucose, 0.9% sodium chloride (equivalent to Na+ 150 mmol/L and Cl- 150 mmol/L); 5% glucose, 0.45% sodium chloride (equivalent to Na+ 75 mmol/L and Cl- 75 mmol/L) [c]. |
| potassium chloride | Solution: 11.2% in 20- mL ampoule
(equivalent to K+ 1.5 mmol/ mL, Cl- 1.5 mmol/ mL). Solution for dilution: 7.5% (equivalent to K 1 mmol/ mL and Cl 1 mmol/ mL) [c]; 15% (equivalent to K 2 mmol/ mL and Cl 2 mmol/ mL) [c]. |
| sodium chloride | Injectable solution: 0.9% isotonic (equivalent to Na+ 154 mmol/L, Cl- 154 mmol/L). |
| sodium hydrogen carbonate | Injectable solution: 1.4% isotonic (equivalent to Na+ 167 mmol/L, HCO3– 167 mmol/L).
Solution: 8.4% in 10- mL ampoule (equivalent to Na+ 1000 mmol/L, HCO3-1000 mmol/L). |
| o sodium lactate, compound solution | Injectable solution. |
| 26.3 Miscellaneous | |
| water for injection | 2- mL; 5- mL; 10- mL ampoules. |
| 27. VITAMINS AND MINERALS | |
| ascorbic acid | Tablet: 50 mg. |
| calcium | Tablet: 500 mg (elemental). |
| colecalciferol [c] | Oral liquid: 400 IU/ mL.
Solid oral dosage form: 400 IU; 1000 IU. * Ergocalciferol can be used as an alternative. |
| o ergocalciferol | Oral liquid: 250 micrograms/ mL (10 000 IU/ mL).
Solid oral dosage form: 1.25 mg (50 000 IU). |
| iodine | Capsule: 200 mg.
Iodized oil: 1 mL (480 mg iodine); 0.5 mL (240 mg iodine) in ampoule (oral or injectable); 0.57 mL (308 mg iodine) in dispenser bottle. |
| o nicotinamide | Tablet: 50 mg. |
| pyridoxine | Tablet: 25 mg (hydrochloride). |
| retinol | Capsule: 50 000 IU; 100 000 IU; 200 000 IU (as palmitate).
Oral oily solution: 100 000 IU (as palmitate)/ mL in multidose dispenser. Tablet (sugar-coated): 10 000 IU (as palmitate). Water-miscible injection: 100 000 IU (as palmitate) in 2- mL ampoule. |
| riboflavin | Tablet: 5 mg. |
| sodium fluoride | In any appropriate topical formulation. |
| thiamine | Tablet: 50 mg (hydrochloride). |
| Complementary List | |
| calcium gluconate | Injection: 100 mg/ mL in 10- mL ampoule. |
| 28. EAR, NOSE AND THROAT MEDICINES [c] | |
| acetic acid | Topical: 2%, in alcohol. |
| o budesonide | Nasal spray: 100 micrograms per dose. |
| o ciprofloxacin | Topical: 0.3% drops (as hydrochloride). |
| o xylometazoline a | Nasal spray: 0.05%.
a Not in children less than 3 months. |
| 29. SPECIFIC MEDICINES FOR NEONATAL CARE | |
| 29.1 Medicines administered to the neonate [c] | |
| caffeine citrate | Injection: 20 mg/ mL (equivalent to 10 mg caffeine base/ mL).
Oral liquid: 20 mg/ mL (equivalent to 10 mg caffeine base/ mL). |
| chlorhexidine | Solution or gel: 7.1% (digluconate) delivering 4% chlorhexidine (for umbilical cord care) [c]. |
| Complementary List | |
| o ibuprofen | Solution for injection: 5 mg/ mL. |
| o prostaglandin E | Solution for injection:
Prostaglandin E1: 0.5 mg/ mL in alcohol. Prostaglandin E 2: 1 mg/ mL. |
| surfactant | Suspension for intratracheal instillation: 25 mg/ mL or 80 mg/ mL. |
| 29.2 Medicines administered to the mother | |
| dexamethasone | Injection: 4 mg/ mL dexamethasone phosphate (as disodium salt) |
| 30. MEDICINES FOR DISEASES OF JOINTS | |
| 30.1 Medicines used to treat gout | |
| allopurinol | Tablet: 100 mg. |
| 30.2 Disease-modifying agents used in rheumatoid disorders (DMARDs) | |
| chloroquine | Tablet: 100 mg; 150 mg (as phosphate or sulfate). |
| Complementary List | |
| azathioprine | Tablet: 50 mg. |
| hydroxychloroquine [c] | Solid oral dosage form: 200 mg (as sulfate). |
| methotrexate | Tablet: 2.5 mg (as sodium salt). |
| penicillamine | Solid oral dosage form: 250 mg. |
| sulfasalazine | Tablet: 500 mg. |
| 30.3 Juvenile joint diseases | |
| acetylsalicylic acid* (acute or chronic use) | Suppository: 50 mg to 150 mg.
Tablet: 100 mg to 500 mg. * For use for rheumatic fever, juvenile arthritis, Kawasaki disease. |
Table 1.1: Medicines with age or weight restrictions
| artesunate + pyronaridine tetraphosphate | > 5 kg |
| atazanavir | >25 kg |
| atropine | >3 months |
| benzyl benzoate | >2 years |
| betamethasone topical preparations | hydrocortisone preferred in neonates |
| cefazolin | >1 month |
| ceftriaxone | >41 weeks corrected gestational age |
| darunavir | > 3 years |
| delamanid | > 6 years |
| dihydroartemisinin + piperaquine phosphate | > 5 kg |
| diloxanide | >25 kg |
| doxycycline | >8 years (except for serious infections e.g. cholera) |
| efavirenz | >3 years or >10 kg |
| fluoxetine | >8 years |
| ibuprofen | >3 months (except IV form for patent ductus arteriosus) |
| mefloquine | >5 kg or >3 months |
| metoclopramide | Not in neonates |
| nevirapine | > 6 weeks |
| ondansetron | >1 month |
| silver sulfadiazine | >2 months |
| tetracaine | Not in preterm neonates |
| trimethoprim | >6 months |
| xylometazoline | >3 months |
Table 1.2: Explanation of dosage forms
A. Principal dosage forms used in EML – oral administration
|
Term |
Definition |
|
Solid oral dosage form |
Refers to tablets or capsules or other solid dosage forms such as ‘melts’ that are immediate-release preparations. It implies that there is no difference in clinical efficacy or safety between the available dosage forms, and countries should therefore choose the form(s) to be listed depending on quality and availability.
The term ‘solid oral dosage form’ is never intended to allow any type of modified-release tablet. |
|
Tablets |
Refers to:
· uncoated or coated (film-coated or sugar-coated) tablets that are intended to be swallowed whole; · unscored and scored*; · tablets that are intended to be chewed before being swallowed; · tablets that are intended to be dispersed or dissolved in water or another suitable liquid before being swallowed; · tablets that are intended to be crushed before being swallowed.
The term ‘tablet’ without qualification is never intended to allow any type of modified-release tablet. |
|
Tablets (qualified) |
Refers to a specific type of tablet:
chewable – tablets that are intended to be chewed before being swallowed; dispersible – tablets that are intended to be dispersed in water or another suitable liquid before being swallowed; soluble – tablets that are intended to be dissolved in water or another suitable liquid before being swallowed; crushable – tablets that are intended to be crushed before being swallowed; scored – tablets bearing a break mark or marks where sub-division is intended in order to provide doses of less than one tablet; sublingual – tablets that are intended to be placed beneath the tongue.
The term ‘tablet’ is always qualified with an additional term (in parentheses) in entries where one of the following types of tablet is intended: gastro-resistant (such tablets may sometimes be described as enteric-coated or as delayed-release), prolonged-release or another modified-release form. |
* Scored tablets may be divided for ease of swallowing, provided that dose is a whole number of tablets.
| Capsules | Refers to hard or soft capsules.
The term ‘capsule’ without qualification is never intended to allow any type of modified-release capsule. |
| Capsules (qualified) | The term ‘capsule’ with qualification refers to gastro-resistant (such capsules may sometimes be described as enteric-coated or as delayed- release), prolonged-release or another modified-release form. |
| Granules | Preparations that are issued to patient as granules to be swallowed without further preparation, to be chewed, or to be taken in or with water or another suitable liquid.
The term ‘granules’ without further qualification is never intended to allow any type of modified-release granules. |
| Oral powder | Preparations that are issued to patient as powder (usually as single- dose) to be taken in or with water or another suitable liquid. |
| Oral liquid | Liquid preparations intended to be swallowed i.e. oral solutions, suspensions, emulsions and oral drops, including those constituted from powders or granules, but not those preparations intended for oromucosal administration e.g. gargles and mouthwashes.
Oral liquids presented as powders or granules may offer benefits in the form of better stability and lower transport costs. If more than one type of oral liquid is available on the same market (e.g. solution, suspension, granules for reconstitution), they may be interchanged and in such cases should be bioequivalent. It is preferable that oral liquids do not contain sugar and that solutions for children do not contain alcohol. |
B. Principal dosage forms used in EML – parenteral administration
| Term | Definition |
| Injection | Refers to solutions, suspensions and emulsions including those
constituted from powders or concentrated solutions. |
| Injection (qualified) | Route of administration is indicated in parentheses where relevant. |
| Injection (oily) | The term `injection’ is qualified by `(oily)’ in relevant entries. |
| Intravenous infusion | Refers to solutions and emulsions including those constituted from
powders or concentrated solutions. |
- Other dosage forms
| Mode of
administration |
Term to be used |
| To the eye | Eye drops, eye ointments. |
| Topical | For liquids: lotions, paints.
For semi-solids: cream, ointment. |
| Rectal | Suppositories, gel or solution. |
| Vaginal | Pessaries or vaginal tablets. |
| Inhalation | Powder for inhalation, pressurized inhalation, nebulizer. |






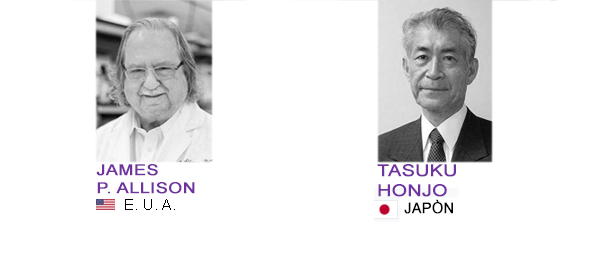

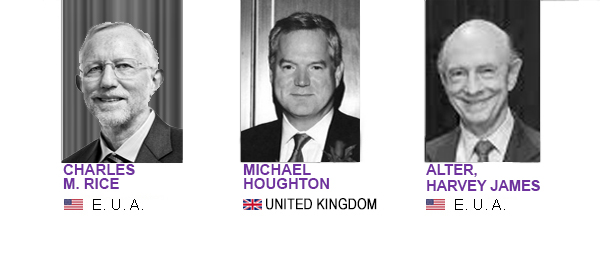




 Escribenos por Whatsapp
Escribenos por Whatsapp